
Join the “Open Your Eyes to UM” Campaign
May 21st, May 22nd and May 23rd
May is Eye Cancer Awareness Month. Ocular Melanoma Ireland (a support group of Irish eye cancer patients and their families), Breakthrough Cancer Research (an Irish medical research charity focused on funding cancer research), and cancer researchers from University College Dublin are raising awareness of Uveal Melanoma, a rare and potentially deadly cancer that develops in the eye. Ireland has one of the highest rates of uveal melanoma in Europe and possibly in the world.
From the 21st through the 23rd of May, people of all ages in Ireland are urged to join our “Open your eyes to UM” campaign.
Uveal melanoma is the most common type of eye cancer in adults. It should not be confused with skin melanoma which differs in its characteristics and treatment. Approximately 50-60 people are diagnosed with uveal melanoma in Ireland each year. Once uveal melanoma is diagnosed, it can be treated by radiation, or occasionally, by the removal of the affected eye. Unfortunately, some uveal melanomas can spread or metastasise to other organs such as the liver. Once this cancer has spread to the liver, it becomes more difficult to treat. Early detection is very important. Uveal melanoma can be treated successfully if caught early.
The importance of routine eye examinations and early discovery of uveal melanoma.
Many people may have a small mole in their eye which is called a “naevus” (plural naevi). Most eye naevi are harmless, but in rare instances, a naevus may develop into a cancer of the eye (melanoma). Routine eye examinations ensure that a naevus will be found, and if it shows any unusual features, it will be monitored. To raise awareness of eye cancer during Eye Cancer Awareness Month, and as part of our “Open your Eyes to UM” campaign, we encourage people of all ages to have routine eye examinations. We are also asking eye care professionals to keep this rare form of cancer in mind when conducting routine eye examinations and to consider using dilation; eye drops that can be given to widen the pupil (the black part of the eye) so that the practitioner can shine a light to see inside to see naevi which would otherwise be difficult to see.
Mr Noel Horgan, a member of the Irish College of Ophthalmologists (ICO) and Consultant Ophthalmologist at the Royal Victoria Eye and Ear Hospital and St Vincent’s University Hospital said:
“If you are aged over 50 or have a family history of eye disease, it is recommended to have a routine eye examination every 1 to 2 years to ensure early diagnosis of any significant eye disorder. In this way some serious eye conditions – such as uveal melanoma can be diagnosed earlier, before symptoms. The ICO encourages people to remember eye health as part of their overall good health and well-being management, particularly as we age and for those in the higher risk categories.”
A patient’s story
Ronan, a married father with three daughters, aged 49, from the northwest,who was diagnosed with uveal melanoma in May, 2018, did have symptoms of the disease. In late December, 2017, he occasionally noticed a bright flash radiating from the corner of his right eye. One month later, in January 2018, the flashes became more frequent, and his wife persuaded him to visit an optometrist. His eyes were examined, but they were not dilated. As he says, “my diagnosis of the flashing lights was put down to high blood pressure.” He was told that his symptoms were due to high blood pressure. Four months later, in May, Ronan his wife noticed that he looked more flushed than usual after jujitsu and suggested that he go to his GP to have his blood pressure checked. 3rd degree black belt, was doing martial arts when he began, as he says, to “turn red”. He went to the He asked the GP to measure his pressure, and also highlighted the flashes. After finding that his blood pressure measurement was normal, the GP advised him to see an optometrist and to have his eyes dilated. The optometrist found “raised pigment” at the back of his eye, and he was referred back to his GP for an emergency referral. The next day, he had a private consultation with an ophthalmologist in Sligo, who diagnosed him with uveal melanoma and referred him for treatment. He says that he had never heard of uveal melanoma and that this diagnosis came as a complete surprise to him.
Treatment at the Royal Victoria Eye and Ear and St Luke’s Hospitals
Mr. Noel Horgan, who specialises in ocular oncology at the Royal Victoria Eye and Ear Hospital and St Vincent’s University Hospital, says that “ocular (eye) tumours occur relatively rarely.” The majority of his patients are given a treatment called plaque brachytherapy, a type of radiation therapy, at St Luke’s Hospital Dublin. Ronan was treated with brachytherapy. Mr. Horgan explains: “Brachytherapy involves treating the tumour within the eye by surgically inserting a radioactive implant (plaque) between the layers around the eye – so the device can deliver radiation locally to treat the tumour inside the eye. That allows the patient to be effectively treated while saving their eye which might otherwise have to be removed.” Patients diagnosed with uveal melanoma are also referred to a consultant medical oncologist for “surveillance” to monitor or keep watch that the cancer has not spread. When uveal melanoma spreads or metastasises to another organ, it most often spreads to the liver, but it can also spread to the lungs or bone. The current treatment options for metastatic uveal melanoma are limited.
Prof John Crown, an internationally renowned medical oncologist and researcher at St Vincent’s University Hospital, in Dublin is heavily involved in follow-up treatments for uveal melanoma patients. He says “I am personally following about 150 patients in my clinics. I have approximately ten consultations, treatments, and ward round visits per week on UM patients. We order approximately 500 imaging scans on UM patients.”
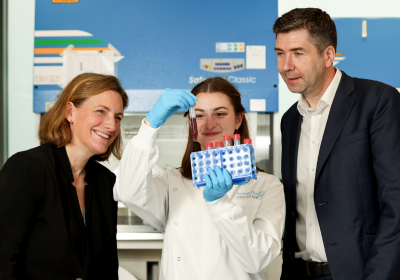
Supporting Research in Ireland
In light of the high incidence of uveal melanoma in Ireland, supporting ongoing research by scientists is critical. Prof John Crown and his team of researchers are building and maintaining international collaborations with colleagues in Southampton, Liverpool and the USA. Prof Breandán Kennedy, who leads uveal melanoma research at the UCD Conway Institute and within a European industry- academia consortium emphasises that, “the need for greater interdisciplinary research into uveal melanoma is indisputable. I want to better understand what causes this cancer and to discover new treatments benefitting uveal melanoma patients in Ireland and worldwide.”
Conclusion
Please “Open your Eyes to UM” and support our eye cancer Awareness campaign this May by attending scheduling a routine eye examinations. The Ocular Melanoma Foundation urges people to seek medical advice if they have any of these typical symptoms: “blurred vision, flashing lights, a shadow in your field of vision”. s and misting of the lens of the eye (cataract)”. If you are diagnosed with eye cancer, or are a family member or carer of someone with eye cancer, please do not hesitate to join the Ocular Melanoma Ireland Facebook support group: OcuMel Irl, and follow @ocumel_irl on twitter.
Donate Now











 Contact
Contact